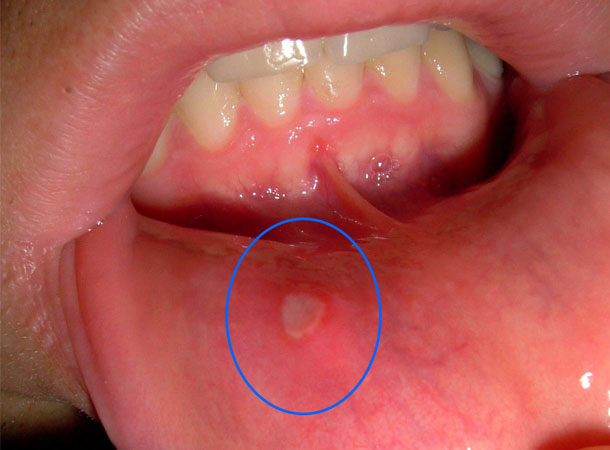
Mouth ulcers can be quite painful and depending on their specific location in the oral cavity, often interfere with your ability to eat and speak. At first, they may appear like a single sore only or in clusters. But, eating certain types of foods can make the condition worse. They may also be found in the soft palate or in the tonsil areas. When they begin to pain, you look for the remedies to heal them.
Given here are home remedies for mouth ulcers that help heal ulcers quickly. Let us have a quick look. But, first let us explore the reason behind the development of these nagging mouth sores.
What Causes Mouth Ulcers?
Any injury like biting the cheek may result in canker sore that pains. When your immune system attacks the healthy cells in your oral cavity instead of harmful microbes then too you are likely to develop these mouth ulcers. Besides, if your diet lacks vitamins, folic acid, iron, B12, zinc etc. you are likely to develop mouth ulcers. Certain types of food allergies (eggs, nuts, coffee, strawberries, etc.) can also result in mouth ulcers. Sometimes emotional stress and hormonal changes, bacterial infection, poor blood circulation or damage done to the gum may also cause canker sores.
Tips for quick pain relief
- If the mouth ulcer is causing a lot of pain, gently rub a small ice cube over the spot or rinse your mouth with ice-cold water.
- You could also chew on a clove bud (lavang) and direct the juice generated to the area where the ulcer is located.
- To prevent the ulcerated area from getting infected, make it a point to rinse your mouth with a little salt water.
Remember, this won’t make the ulcer disappear, but it can help reduce the pain.
While the above are short-term tips to give you relief from ulcer pain, the below-mentioned ingredients are remedies that will help you get rid of them.
1. Honey
Honey is a natural humectant – that is, it helps retain moisture and prevent dehydration. It also helps reduce scarring and hastens the process of new tissue growth. This, along with its anti-microbial effect ensures faster healing of the mouth ulcer. Tip: Dab a little honey onto the mouth ulcer or mix in a little turmeric to make a paste that can be applied on the affected area.
2. Tulsi
Leaves of tulsi plant have amazing medicinal properties and one of the important actions of tulsi is as an adaptogen – a substance that aids the body to adapt to stress. Tip: Chew a few leaves of tulsi along with some water about three to four times every day. This will help in getting rid of ulcers faster and also have a preventive action against their recurrence.
3. Coconut
Dry coconut, coconut oil and coconut water are three products of the coconut tree that are very useful in treating mouth ulcers. Tip: Drinking tender coconut water helps to cool the body. Applying a little coconut oil directly onto the mouth ulcer or chewing some coconut (fresh or dry) helps reduce pain and inflammation and hence, ulcers heal faster.
4. Poppy Seeds
Poppy seeds or khus-khus are said to have a cooling effect on the body. According to Ayurveda, too much heat in the body manifests as mouth ulcers and therefore, poppy seeds are a good remedy to overcome this problem. Tip: Mix some sugar to crushed khus-khus seeds and consume this mixture for instant relief from ulcers. Read more about .
5. Tumeric
External application of turmeric solution helps cure mouth sores. Turmeric is a natural antiseptic and a great cooling agent. The suspension of turmeric is used for gargling if the sores are in the throat region.
Other cooling agents
In keeping with the logic that mouth ulcers are due to excess body heat, other substances with cooling properties can help get rid of them. For example, you could apply a little ghee directly to the ulcerated area, or drink a glass of buttermilk two or three times every day. Castor oil also has wonderful cooling property; apply a little oil to your scalp and the soles of the feet, allow the oil to soak in for a few hours and then wash with warm water.
Word of caution: Mouth ulcers left untreated generally go away in a week or so; with these home remedies, you can expect faster relief. However, if you notice an ulcer in the mouth that is persistently present although it does not cause you any pain, do not neglect it or try to treat it with home remedies beyond a few days. Make it a point to see a doctor soon because often, a painless mouth ulcer is one of the earliest signs of oral cancer.