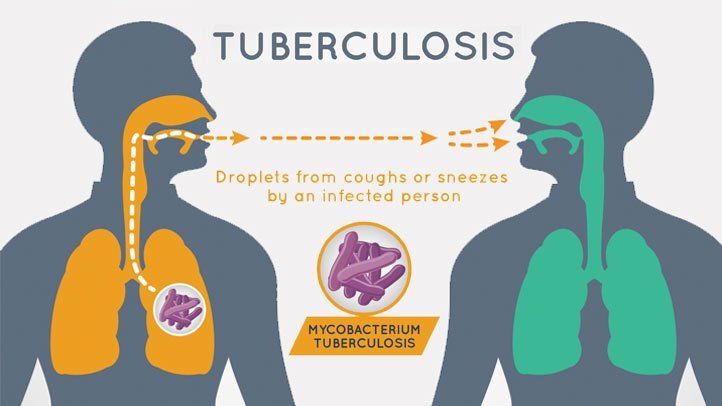
Tuberculosis is a contagious infection that usually attacks our lungs. It is caused by infection with Mycobacterium Tuberculosis (Mtb). Tb can be fatal ,but in many cases , it is preventable as well as treatable. It can develop when bacteria spread through droplets in the air.
Globally , Tuberculosis is a major public health problem.Despite the long history of tuberculosis prevention efforts ,it still ranks among the top ten causes of death in Nepal.In the 20th century Tb was a leading cause of death in the United States. Today,most cases are cured with the help of Antibiotics.But it requires a long time .We need to take medication for at least 6 to 9 months .There are two types of Tuberculosis.
1. Latent Tuberculosis
2. Active Tuberculosis:
Latent Tuberculosis:
You don’t have any symptoms ,but the infection is still alive and can one day become active.You have the germs in your body ,but your immune system keeps them from spreading.If you are at high risk for re-activation for instance ,if you have HIV, you had an infection in past 2years ,your chest X-ray is unusual or your immune system is weakened your doctor will give you medication to prevent.
Active Tuberculosis:
The germs multiply and make you sick. You can spread the disease to others. Ninety percent of active cases in adults come from a latent TB infection.
A latent or active TB infection can also be drug-resistant, meaning certain medications don’t work against the bacteria.
Latent TB doesn’t have symptoms. A skin or blood test can tell if you have it.
General Symptoms :
- A cough that lasts more than 3 weeks
- Chest pain
- Coughing up blood
- Feeling tired all the time
- Night sweats
- Chills
- Fever
- Loss of appetite
- Weight loss
TB Prevention – Precautions, masks & vaccines:
Firstly there is a need to stop the transmission of TB from one adult to another.
This is done through firstly, identifying people with active TB, and then curing them through the provision of drug treatment. With proper TB treatment someone with TB will very quickly not be infectious and so can no longer spread TB to others
.
If someone is not on treatment, then precautions such as cough etiquette, must be taken to prevent TB spreading from one adult to another.
Anything which increases the number of people infected by each infectious person, such as ineffective treatment because of drug resistant TB, reduces the overall effect of the main TB prevention efforts. The presence of TB and HIV infection together also increases the number of people infected by each infectious person. As a result it is then more likely that globally the number of people developing active TB will increase rather than decrease.
Other TB prevention activities:
There are several other TB prevention activities. This includes preventing people with latent TB from developing active, and infectious, TB disease.
TB infection control including the use of masks & respirators, which means preventing the transmission of TB in such settings as hospitals & prisons.
The pasteurization of milk also helps to prevent humans from getting bovine TB.
There is a vaccine for TB, but it makes only a small contribution to TB prevention. It does little to interrupt the transmission of TB among adults.
TB Prevention – the BCG vaccine:
The vaccine called Bacillus Calmette-Guerin (BCG) was first developed in the 1920s. It is one of the most widely used of all current vaccines, and it reaches more than 80% of all newborn children and infants in countries where it is part of the national childhood immunization programme.2 However, it is also one of the most variable vaccines in routine use.
The BCG vaccine has been shown to provide children with excellent protection against the disseminated forms of TB. However protection against pulmonary TB in adults is variable. Since most transmission originates from adult cases of pulmonary TB, the BCG vaccine is generally used to protect children, rather than to interrupt transmission among adults.
The BCG vaccine will often result in the person vaccinated having a positive result to a TB skin test.
TB education:
TB education is necessary for people with TB. People with TB need to know how to take their TB drugs properly. They also need to know how to make sure that they do not pass TB on to other people. But TB education is also necessary for the general public. The public needs to know basic information about TB for a number of reasons including reducing the stigma still associated with TB.
TB treatment as TB prevention:
TB drug treatment for the prevention of TB, also known as chemoprophylaxis, can reduce the risk of a first episode of active TB occurring in people with latent TB. The treatment of latent TB is being used as a tool to try and eliminate TB in the United States.
Isoniazid is one of the drugs used to prevent latent TB from progressing to active TB or TB disease. Isoniazid is a cheap drug, but in a similar way to the use of the BCG vaccine, it is mainly used to protect individuals rather than to interrupt transmission between adults. This is because children rarely have infectious TB, and it is hard to administer isoniazid on a large scale to adults who do not have any symptoms. Taking isoniazid daily for six months is difficult in respect of adherence, and as a result many individuals who could benefit from the treatment, stop taking the drug before the end of the six month period.
There have also been concerns about the possible impact of TB treatment for prevention programmes on the emergence of drug resistance. However, a review of the scientific evidence has now shown that there is no need for this to be a concern. The benefit of isoniazid preventive therapy for people living with HIV, and who have, or may have had latent TB, has also recently been emphasized.
National Tuberculosis Program : Bhaktapur
The National Tuberculosis Program (NTP) is fully integrated within the general primary health care system of the Government of Nepal. The National Tuberculosis Control Centre (NTCC) is the focal point of the NTP. It is responsible for formulating program policies, strategy and planning.
Central laboratory at the NTCC is the focal point for the NTP laboratory network, which is responsible for policy and guideline development, training, quality control and supervision. Technical support, monitoring and evaluation, training, supervision, logistics, health education, communication, and research are key functions of NTCC.
Furthermore, quantification and procurement and supply of anti-tuberculosis drugs are key responsibilities of the NTCC. The NTCC is procuring both first and second line anti TB drugs for the TB patients from Global Drug Facility (GDF). Drugs are distributed through the system of Logistics Management Division of the Department of Health Services. NTCC has also established a Program Management Unit (PMU) at the central level for overall management of the Global Fund grants and provides technical inputs to formulate policies, program, implementation, monitoring and evaluation for the program.
At the Regional level, NTP activities are planned and carried out in coordination and cooperation with the Regional Health Directorate. The Regional Tuberculosis Centre (RTC) in Pokhara provides technical support to TB control activities in the Western Region in coordination with NTCC. There are full time permanent Regional TB Leprosy Officers (RTLO) appointed in each region. Regional levels are responsible for program implementation within the regions. In addition, the regional office is responsible for training, monitoring & evaluation and supervision of program activities. Regional office also provides logistical support, supply of TB drugs and other requirements through Regional Logistic Management Division.
World Tuberculosis Day was marked here today with the theme ‘Wanted: leaders for a TB-free world’.
“It is an effort to end TB” said Dr Kedar Narsingh KC, director at National Tuberculosis Center.
To meet the Sustainable Development Goals, Nepal has to eradicate TB by 2030, however, increasing cases of multidrug resistant TB have turned out to be a major hurdle in achieving SDGS.
Health practitioners themselves are suffering from multi-drug resistant tuberculosis. It is estimated that there are 1,000 MDR-TB cases in the country. From among 1,000 patients only 400 are receiving treatment through DOTS centres under the National Tuberculosis Programme, according to Dr KC.
Multidrug resistant tuberculosis is a form of tuberculosis infection caused by bacteria that are resistant to treatment with at least two of the most powerful first-line anti-TB medications. “The tendency of TB patients dropping out of treatment is increasing as the treatment course spans over 24 months. Irregular medication among TB patients leads to resistance to first-line anti-TB medications. These patients are ultimately diagnosed with MDR-TB,” said Dr KC.
The World Health Organisation estimates that there were 600,000 new cases with resistance to rifampicin, the most effective first-line drug, of which 490,000 had MDR-TB. Along with the multi-drug resistant patients there are at least 11,000 to 13,000 patients who are not seeking any treatment. It is estimated that some 45,000 new cases of tuberculosis are added each year. As per National Tuberculosis Centre, in 2016/17, a total of 31,764 cases were registered under National Tuberculosis Programme.
Anti-Tuberculosis Association(NATA) : Kalimati
Nepal Anti Tuberculosis Association (NATA) is a non-governmental, non-profit making social voluntary organization established in 1953 A.D. with a view to promoting tuberculosis control programs through raising public awareness and adopting preventive and curative measures.
NATA is registered with the District Administration Office in Kathmandu. NATA is affiliated to International Union Against Tuberculosis and Lung Disease (The Union) and Social Welfare Council (SWC), Nepal. It is also one of the prominent members of the South East Asian Region (SEAR).
NATA has a long history of close coordination and collaboration with the National Tuberculosis Programme (NTP), ministry of health as one of the oldest key partners. NATA has been playing an active role in controlling TB to the best of its capacity by expanding and making its preventive and curative services more effective in line with national policies and strategies through mobilization of its 35 district branches and active volunteers in close coordination and co-operation with various local, national and international organizations.
Objectives:
To help the patients of Tuberculosis and Lungs disease in all possible ways
To generate public awareness about the menace of TB and other diseases like Lungs, HIV, etc. through various awareness raising campaigns.
To study the problems of TB in Nepal and adopt various measures (preventive and curative) for the control of diseases.
To make curative service accessible and affordable to marginalized, underprivileged and unreached population affected by TB ensuring the quality of service
To conduct study and research activities on scientific and social aspects of TB
To support National Tuberculosis Control Program to fight against Tuberculosis in Nepal
To seek friendly cooperation and mutual exchange of ideas among various institutions, associations and organizations devoted to anti-TB work all over the world.
To provide all types of curative facilities for the treatment of tuberculosis and other lungs related diseases.
Reference:
http://nepalntp.gov.np
https://www.webmd.com/lung/understanding-tuberculosis-basics
https://www.tbalert.org/about-tb/what-is-tb/prevention/